Binder, J; Palmrich, P; Kalafat, E; Haberl, C; Schirwani, N; Pateisky, P; Khalil, A
(2023)
Longitudinal assessment of angiogenic markers in prediction of adverse outcome in women with confirmed pre-eclampsia.
Ultrasound Obstet Gynecol, 62 (6).
pp. 843-851.
ISSN 1469-0705
https://doi.org/10.1002/uog.26276
SGUL Authors: Khalil, Asma
|
PDF
Published Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (1MB) | Preview |
|
![[img]](https://openaccess.sgul.ac.uk/115695/11.hassmallThumbnailVersion/uog26276-sup-0001-figures1.jpg)
|
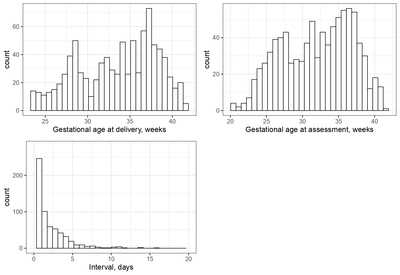
Image (JPEG) (Figure S1)
Published Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (279kB) | Preview |
|
|
Microsoft Word (.docx) (Tables S1-S3)
Published Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (41kB) |
||
|
PDF
Accepted Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (2MB) | Preview |
Abstract
OBJECTIVES: Angiogenic marker assessment, such as the ratio of soluble fms-like tyrosine kinase-1 (sFlt-1) to placental growth factor (PlGF), is known to be a useful tool in the prediction of pre-eclampsia (PE). However, evidence from surveillance strategies in pregnancies with a PE diagnosis is lacking. Therefore, we aimed to assess the predictive performance of longitudinal maternal serum angiogenic marker assessment for both maternal and perinatal adverse outcomes when compared to standard laboratory parameters in pregnancies with confirmed PE. METHODS: This was a retrospective analysis of prospectively collected data from January 2013 to December 2020 at the Medical University of Vienna. The inclusion criteria were singleton pregnancy with confirmed PE and post-diagnosis maternal serum angiogenic marker assessment at a minimum of two timepoints. The primary outcome was the predictive performance of longitudinal sFlt-1 and PlGF assessment for adverse maternal and perinatal outcomes compared to conventional laboratory monitoring at the same time in pregnancies with confirmed PE. Composite adverse maternal outcome included intensive care unit admission, pulmonary edema, eclampsia and/or death. Composite adverse perinatal outcome included stillbirth, neonatal death, placental abruption, neonatal intensive care unit admission, intraventricular hemorrhage, necrotizing enterocolitis, respiratory distress syndrome and/or mechanical ventilator support. RESULTS: In total, 885 post-diagnosis sFlt-1/PlGF ratio measurements were obtained from 323 pregnant women with confirmed PE. For composite adverse maternal outcome, the highest standalone predictive accuracy was obtained using maternal serum sFlt-1/PlGF ratio (area under the receiver-operating-characteristics curve (AUC), 0.72 (95% CI, 0.62-0.81)), creatinine (AUC, 0.71 (95% CI, 0.62-0.81)) and lactate dehydrogenase (LDH) levels (AUC, 0.73 (95% CI, 0.65-0.81)). Maternal platelet levels (AUC, 0.65 (95% CI, 0.55-0.74)), serum alanine aminotransferase (ALT) (AUC, 0.59 (95% CI, 0.49-0.69)) and aspartate aminotransferase (AST) (AUC, 0.61 (95% CI, 0.51-0.71) levels had poor standalone predictive accuracy. The best prediction model consisted of a combination of maternal serum LDH, creatinine levels and sFlt-1/PlGF ratio, which had an AUC of 0.77 (95% CI, 0.68-0.85), significantly higher than sFlt-1/PlGF ratio alone (P = 0.037). For composite adverse perinatal outcome, the highest standalone predictive accuracy was obtained using maternal serum sFlt-1/PlGF ratio (AUC, 0.82 (95% CI, 0.75-0.89)) and creatinine (AUC, 0.74 (95% CI, 0.67-0.80)) levels, sFlt-1/PlGF ratio being superior to creatinine alone (P < 0.001). Maternal serum LDH levels (AUC, 0.65 (95% CI, 0.53-0.74)), platelet count (AUC, 0.57 (95% CI, 0.44-0.67)), ALT (AUC, 0.58 (95% CI, 0.48-0.67)) and AST (AUC, 0.58 (95% CI, 0.48-0.67)) levels had poor standalone predictive accuracy. No combination of biomarkers was superior to maternal serum sFlt-1/PlGF ratio alone for prediction of composite adverse perinatal outcome (P > 0.05 for all). CONCLUSIONS: In pregnancies with confirmed PE, longitudinal maternal serum angiogenic marker assessment is a good predictor of adverse maternal and perinatal outcomes and superior to some conventional laboratory parameters. Further studies should focus on optimal surveillance following diagnosis of PE. © 2023 The Authors. Ultrasound in Obstetrics & Gynecology published by John Wiley & Sons Ltd on behalf of International Society of Ultrasound in Obstetrics and Gynecology.
Statistics
Actions (login required)
 |
Edit Item |