Estcourt, CS;
Gibbs, J;
Gkatzidou, V;
Sutcliffe, LJ;
Tickle, L;
Hone, K;
Aicken, CR;
Lowndes, CM;
Harding-Esch, EM;
Eaton, S;
et al.
Estcourt, CS; Gibbs, J; Gkatzidou, V; Sutcliffe, LJ; Tickle, L; Hone, K; Aicken, CR; Lowndes, CM; Harding-Esch, EM; Eaton, S; Oakeshott, P; Szczepura, A; Ashcroft, RE; Copas, A; Nettleship, A; Sonnenberg, P; Sadiq, ST
(2017)
The eSexual Health Clinic system for management, prevention, and control of sexually transmitted infections: exploratory studies in people testing for Chlamydia trachomatis.
Lancet Public Health, 2 (4).
e182-e190.
https://doi.org/10.1016/S2468-2667(17)30034-8
SGUL Authors: Harding-Esch, Emma Michele Oakeshott, Philippa
|
PDF
Published Version
Available under License Creative Commons Attribution. Download (979kB) | Preview |
|
|
Microsoft Word (.docx)
Accepted Version
Available under License Creative Commons Attribution. Download (571kB) |
||
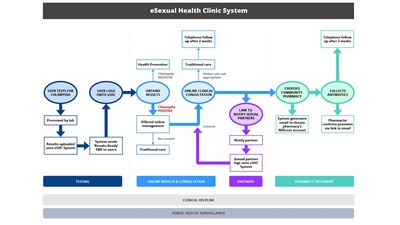
![[img]](https://openaccess.sgul.ac.uk/108597/3.hassmallThumbnailVersion/Figure%201.jpg)
|
Image (JPEG) (Figure 1)
Accepted Version
Available under License Creative Commons Attribution. Download (1MB) | Preview |
|
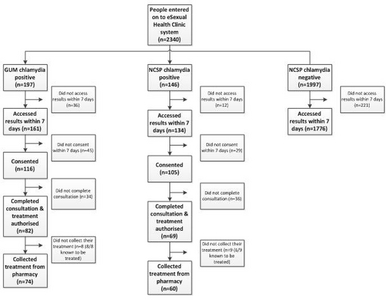
![[img]](https://openaccess.sgul.ac.uk/108597/11.hassmallThumbnailVersion/Figure%202.jpg)
|
Image (JPEG) (Figure 2)
Accepted Version
Available under License Creative Commons Attribution. Download (1MB) | Preview |
Abstract
Background Self-directed and internet-based care are key elements of eHealth agendas. We developed a complex online clinical and public health intervention, the eSexual Health Clinic (eSHC), in which patients with genital chlamydia are diagnosed and medically managed via an automated online clinical consultation, leading to antibiotic collection from a pharmacy. Partner notification, health promotion, and capture of surveillance data are integral aspects of the eSHC. We aimed to assess the safety and feasibility of the eSHC as an alternative to routine care in non-randomised, exploratory proof-of-concept studies. Methods Participants were untreated patients with chlamydia from genitourinary medicine clinics, untreated patients with chlamydia from six areas in England in the National Chlamydia Screening Programme's (NCSP) online postal testing service, or patients without chlamydia tested in the same six NCSP areas. All participants were aged 16 years or older. The primary outcome was the proportion of patients with chlamydia who consented to the online chlamydia pathway who then received appropriate clinical management either exclusively through online treatment or via a combination of online management and face-to-face care. We captured adverse treatment outcomes. Findings Between July 21, 2014, and March 13, 2015, 2340 people used the eSHC. Of 197 eligible patients from genitourinary medicine clinics, 161 accessed results online. Of the 116 who consented to be included in the study, 112 (97%, 95% CI 91–99) received treatment, and 74 of those were treated exclusively online. Of the 146 eligible NCSP patients, 134 accessed their results online, and 105 consented to be included. 93 (89%, 95% CI 81–94) received treatment, and 60 were treated exclusively online. In both groups, median time to collection of treatment was within 1 day of receiving their diagnosis. 1776 (89%) of 1936 NCSP patients without chlamydia accessed results online. No adverse events were recorded. Interpretation The eSHC is safe and feasible for management of patients with chlamydia, with preliminary evidence of similar treatment outcomes to those in traditional services. This innovative model could help to address growing clinical and public health needs. A definitive trial is needed to assess the efficacy, cost-effectiveness, and public health impact of this intervention. Funding UK Clinical Research Collaboration.
| Item Type: | Article | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Additional Information: | © The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY license. | ||||||||
| SGUL Research Institute / Research Centre: | Academic Structure > Population Health Research Institute (INPH) | ||||||||
| Journal or Publication Title: | Lancet Public Health | ||||||||
| Publisher License: | Creative Commons: Attribution 4.0 | ||||||||
| Projects: |
|
||||||||
| Dates: |
|
||||||||
| URI: | https://openaccess.sgul.ac.uk/id/eprint/108597 | ||||||||
| Publisher's version: | https://doi.org/10.1016/S2468-2667(17)30034-8 |
Statistics
Actions (login required)
 |
Edit Item |