Geier, CB;
Ellison, M;
Cruz, R;
Pawar, S;
Leiss-Piller, A;
Zmajkovicova, K;
McNulty, SM;
Yilmaz, M;
Evans, MO;
Gordon, S;
et al.
Geier, CB; Ellison, M; Cruz, R; Pawar, S; Leiss-Piller, A; Zmajkovicova, K; McNulty, SM; Yilmaz, M; Evans, MO; Gordon, S; Ujhazi, B; Wiest, I; Abolhassani, H; Aghamohammadi, A; Barmettler, S; Bhar, S; Bondarenko, A; Bolyard, AA; Buchbinder, D; Cada, M; Cavieres, M; Connelly, JA; Dale, DC; Deordieva, E; Dorsey, MJ; Drysdale, SB; Ehl, S; Elfeky, R; Fioredda, F; Firkin, F; Förster-Waldl, E; Geng, B; Goda, V; Gonzalez-Granado, L; Grunebaum, E; Grzesk, E; Henrickson, SE; Hilfanova, A; Hiwatari, M; Imai, C; Ip, W; Jyonouchi, S; Kanegane, H; Kawahara, Y; Khojah, AM; Kim, VH-D; Kojić, M; Kołtan, S; Krivan, G; Langguth, D; Lau, Y-L; Leung, D; Miano, M; Mersyanova, I; Mousallem, T; Muskat, M; Naoum, FA; Noronha, SA; Ouederni, M; Ozono, S; Richmond, GW; Sakovich, I; Salzer, U; Schuetz, C; Seeborg, FO; Sharapova, SO; Sockel, K; Volokha, A; von Bonin, M; Warnatz, K; Wegehaupt, O; Weinberg, GA; Wong, K-J; Worth, A; Yu, H; Zharankova, Y; Zhao, X; Devlin, L; Badarau, A; Csomos, K; Keszei, M; Pereira, J; Taveras, AG; Beaussant-Cohen, SL; Ong, M-S; Shcherbina, A; Walter, JE
(2022)
Disease Progression of WHIM Syndrome in an International Cohort of 66 Pediatric and Adult Patients.
J Clin Immunol, 42 (8).
pp. 1748-1765.
ISSN 1573-2592
https://doi.org/10.1007/s10875-022-01312-7
SGUL Authors: Drysdale, Simon Bruce
|
PDF
Published Version
Available under License Creative Commons Attribution. Download (2MB) | Preview |
|
![[img]](https://openaccess.sgul.ac.uk/114663/6.hassmallThumbnailVersion/10875_2022_1312_MOESM1_ESM.png)
|
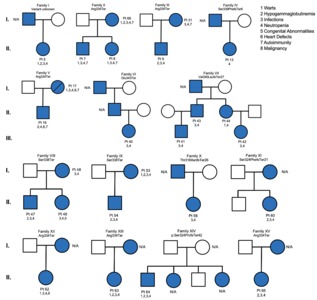
Image (PNG) (Supplementary Figure 1)
Published Version
Available under License Creative Commons Attribution. Download (263kB) | Preview |
|
|
Image (TIFF) (Supplementary Figure 2)
Published Version
Available under License Creative Commons Attribution. Download (5MB) | Preview |
|
![[img]](https://openaccess.sgul.ac.uk/114663/19.hassmallThumbnailVersion/10875_2022_1312_Fig6_ESM.png)
|
Image (PNG) (High Resolution Image)
Published Version
Available under License Creative Commons Attribution. Download (569kB) | Preview |
|
|
Microsoft Excel (Supplementary Table 1)
Published Version
Available under License Creative Commons Attribution. Download (17kB) |
||
|
Microsoft Excel (Supplementary Table 2)
Published Version
Available under License Creative Commons Attribution. Download (20kB) |
||
|
Microsoft Word (.docx) (Supplementary Table 3)
Published Version
Available under License Creative Commons Attribution. Download (15kB) |
||
|
Microsoft Excel (Supplementary Table 4)
Published Version
Available under License Creative Commons Attribution. Download (11kB) |
Abstract
Warts, hypogammaglobulinemia, infections, and myelokathexis (WHIM) syndrome (WS) is a combined immunodeficiency caused by gain-of-function mutations in the C-X-C chemokine receptor type 4 (CXCR4) gene. We characterize a unique international cohort of 66 patients, including 57 (86%) cases previously unreported, with variable clinical phenotypes. Of 17 distinct CXCR4 genetic variants within our cohort, 11 were novel pathogenic variants affecting 15 individuals (23%). All variants affect the same CXCR4 region and impair CXCR4 internalization resulting in hyperactive signaling. The median age of diagnosis in our cohort (5.5 years) indicates WHIM syndrome can commonly present in childhood, although some patients are not diagnosed until adulthood. The prevalence and mean age of recognition and/or onset of clinical manifestations within our cohort were infections 88%/1.6 years, neutropenia 98%/3.8 years, lymphopenia 88%/5.0 years, and warts 40%/12.1 years. However, we report greater prevalence and variety of autoimmune complications of WHIM syndrome (21.2%) than reported previously. Patients with versus without family history of WHIM syndrome were diagnosed earlier (22%, average age 1.3 years versus 78%, average age 5 years, respectively). Patients with a family history of WHIM syndrome also received earlier treatment, experienced less hospitalization, and had less end-organ damage. This observation reinforces previous reports that early treatment for WHIM syndrome improves outcomes. Only one patient died; death was attributed to complications of hematopoietic stem cell transplantation. The variable expressivity of WHIM syndrome in pediatric patients delays their diagnosis and therapy. Early-onset bacterial infections with severe neutropenia and/or lymphopenia should prompt genetic testing for WHIM syndrome, even in the absence of warts.
| Item Type: | Article | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Additional Information: | © The Author(s) 2022 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. | ||||||||||||
| Keywords: | CXCR4, autoimmunity, lymphopenia, myelokathexis, neutropenia, warts, 1107 Immunology, Immunology | ||||||||||||
| SGUL Research Institute / Research Centre: | Academic Structure > Infection and Immunity Research Institute (INII) | ||||||||||||
| Journal or Publication Title: | J Clin Immunol | ||||||||||||
| ISSN: | 1573-2592 | ||||||||||||
| Language: | eng | ||||||||||||
| Dates: |
|
||||||||||||
| Publisher License: | Creative Commons: Attribution 4.0 | ||||||||||||
| Projects: |
|
||||||||||||
| PubMed ID: | 35947323 | ||||||||||||
 |
Go to PubMed abstract | ||||||||||||
| URI: | https://openaccess.sgul.ac.uk/id/eprint/114663 | ||||||||||||
| Publisher's version: | https://doi.org/10.1007/s10875-022-01312-7 |
Statistics
Actions (login required)
 |
Edit Item |