Chimhini, G;
Chimhuya, S;
Madzudzo, L;
Heys, M;
Crehan, C;
Robertson, V;
Ferrand, RA;
Sado, B;
Sharland, M;
Walker, AS;
et al.
Chimhini, G; Chimhuya, S; Madzudzo, L; Heys, M; Crehan, C; Robertson, V; Ferrand, RA; Sado, B; Sharland, M; Walker, AS; Klein, N; Fitzgerald, FC
(2020)
Auditing use of antibiotics in Zimbabwean neonates.
Infect Prev Pract, 2 (2).
p. 100046.
ISSN 2590-0889
https://doi.org/10.1016/j.infpip.2020.100046
SGUL Authors: Sharland, Michael Roy
|
PDF
Published Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (255kB) | Preview |
|
|
Microsoft Word (.docx) (Supplementary material 1)
Published Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (23kB) |
||
![[img]](https://openaccess.sgul.ac.uk/113583/8.hassmallThumbnailVersion/1-s2.0-S259008892030010X-figs1.jpg)
|
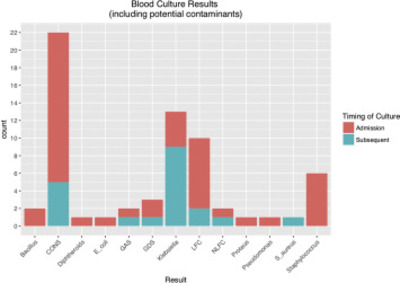
Image (JPEG) (Supplementary material 2)
Published Version
Available under License Creative Commons Attribution Non-commercial No Derivatives. Download (19kB) | Preview |
Abstract
Background: Neonatal sepsis is a major cause of morbidity and mortality in low-income settings. As signs of sepsis are non-specific and deterioration precipitous, antibiotics are often used profusely in these settings where diagnostics may not be readily available. Harare Central Hospital, Zimbabwe, delivers 12000 babies per annum admitting ∼4800 to the neonatal unit. Overcrowding, understaffing and rapid staff turnover are consistent problems. Suspected sepsis is highly prevalent, and antibiotics widely used. We audited the impact of training and benchmarking intervention on rationalizing antibiotic prescription using local, World Health Organization-derived, guidelines as the standard. Methods: An initial audit of admission diagnosis and antibiotic use was performed between 8th May - 6th June 2018 as per the audit cycle. An intern training programme, focusing on antimicrobial stewardship and differentiating between babies 'at risk of' versus 'with' clinically-suspected sepsis was instituted post-primary audit. Re-audit was conducted after 5 months. Results: Sepsis was the most common admitting diagnosis by interns at both time points but reduced at repeat audit (81% versus 59%, P<0.0001). Re-audit after 5 months demonstrated a decrease in antibiotic prescribing at admission and discharge. Babies prescribed antibiotics at admission decreased from 449 (98%) to 96 (51%), P<0.0001. Inpatient days of therapy (DOT) reduced from 1243 to 1110/1000 patient-days. Oral amoxicillin prescription at discharge reduced from 349/354 (99%) to 1% 1/161 (P<0.0001). Conclusion: A substantial decrease in antibiotic use was achieved by performance feedback, training and leadership, although ongoing performance review will be key to ensuring safety and sustainability.
| Item Type: | Article | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Additional Information: | © 2020 The Authors. Published by Elsevier Ltd on behalf of The Healthcare Infection Society. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/). | |||||||||
| Keywords: | Antibiotics, Antimicrobial stewardship, Low-income setting, Neonatal sepsis, Neonatal unit, Zimbabwe | |||||||||
| SGUL Research Institute / Research Centre: | Academic Structure > Infection and Immunity Research Institute (INII) | |||||||||
| Journal or Publication Title: | Infect Prev Pract | |||||||||
| ISSN: | 2590-0889 | |||||||||
| Language: | eng | |||||||||
| Dates: |
|
|||||||||
| Publisher License: | Creative Commons: Attribution-Noncommercial-No Derivative Works 4.0 | |||||||||
| Projects: |
|
|||||||||
| PubMed ID: | 34368696 | |||||||||
 |
Go to PubMed abstract | |||||||||
| URI: | https://openaccess.sgul.ac.uk/id/eprint/113583 | |||||||||
| Publisher's version: | https://doi.org/10.1016/j.infpip.2020.100046 |
Statistics
Actions (login required)
 |
Edit Item |